Doctor and patient reviewing an advanced lipid report
If you’ve ever looked at your cholesterol results and thought, “My LDL is fine, so why is my doctor still concerned?”, you’re not alone. The confusion often comes from mixing up LDL-C with LDL particle number (LDL-P).
Here’s the practical bottom line: LDL-C tells you how much cholesterol is being carried, while LDL-P tells you how many LDL “carriers” are circulating. When those two don’t match, risk can be misread, especially in people with higher triglycerides or insulin resistance.
This guide breaks down the difference, when LDL-P is usually ordered, and a simple 3-week food focus that supports better numbers without turning life into a diet spreadsheet.
LDL-C vs LDL particle number (LDL-P): two ways to describe the same “traffic”
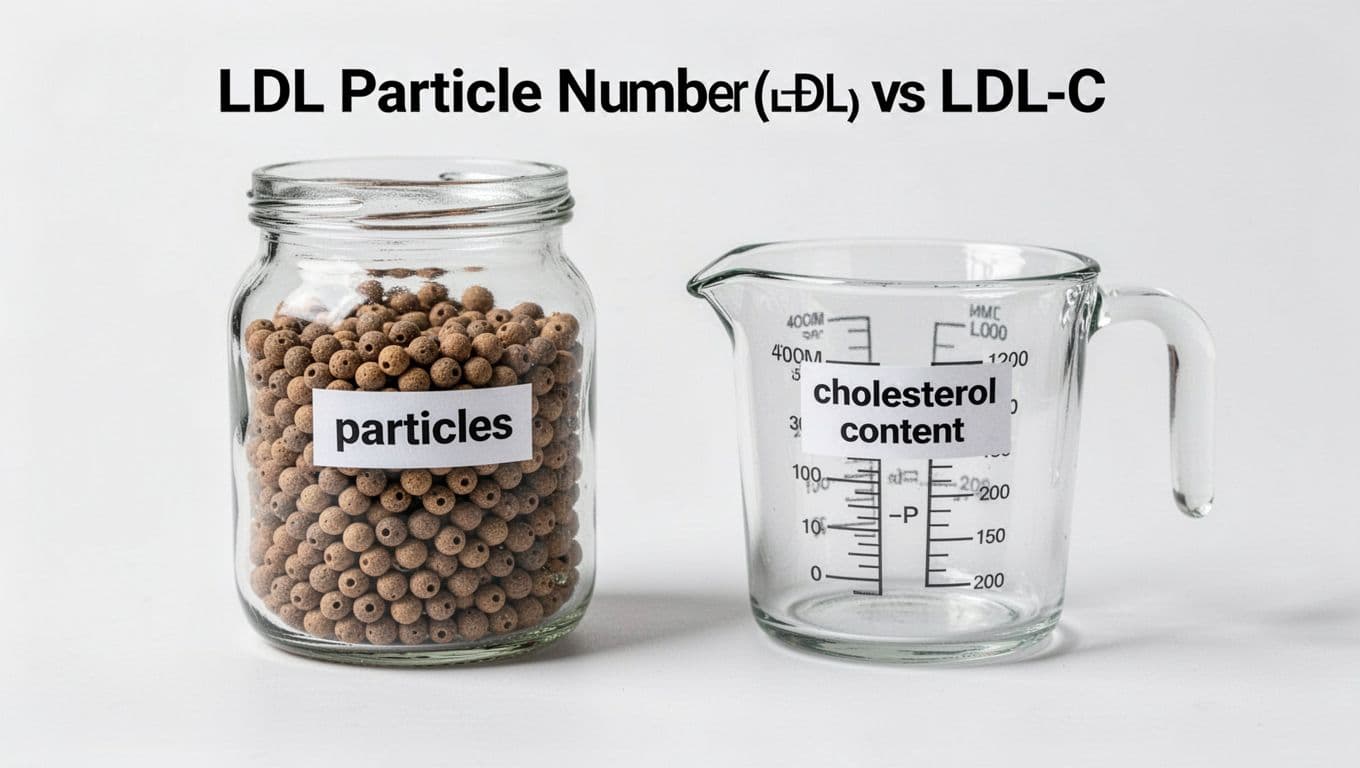
Two props that show “count” vs “amount”
Think of LDL particles like cars on a highway. LDL-C is the total amount of “cargo” (cholesterol) inside all the cars. LDL-P is the number of cars on the road. Even if the cargo looks modest, more cars means more chances for traffic to clog the artery wall over time.
This mismatch is called discordance. It’s common when triglycerides run high, when blood sugar runs high, or when someone has a pattern tied to insulin resistance. In those cases, each LDL particle may carry less cholesterol, so LDL-C can look “okay” while LDL-P stays high.
A related marker is ApoB, which also reflects particle count. If you want the clearest plain-English bridge between these tests, this internal guide on particle count vs cholesterol content makes the “how many boats vs how much cargo” idea stick.
Here’s a quick comparison to keep on hand:
| Test on your report | What it measures | Why it can matter |
|---|---|---|
| LDL-C | Cholesterol mass inside LDL particles | Helpful treatment target, but can miss discordance |
| LDL-P | Number of LDL particles (often via NMR) | Often tracks risk better when LDL-C and risk don’t match |
| ApoB | Count of atherogenic particles (one ApoB per particle) | Practical particle “headcount,” includes more than LDL |
When you hear “advanced lipid testing,” LDL-P is usually what people mean.
When doctors order LDL-P (and what they’re trying to learn)
LDL-P is not a routine add-on for every annual physical. Doctors usually order it when a standard lipid panel leaves too many unanswered questions.
Common reasons include:
- A strong family history of early heart disease, especially if LDL-C seems “not that bad.”
- Metabolic syndrome, prediabetes, or type 2 diabetes, where particle patterns often shift.
- High triglycerides, fatty liver, or extra abdominal weight, because these often travel with smaller, more numerous particles.
- Unexpected results after lifestyle changes or medication, when the “headline” LDL-C falls but risk still feels unclear.
LDL-P is commonly measured by NMR lipoprotein testing. Results are usually reported in nmol/L, which can look unfamiliar. Some clinician resources use practical cut points (for example, under about 1200 nmol/L as a lower-risk range, and higher numbers signaling more concern), but your target depends on your full risk picture.
If LDL-P is high, it’s not a character flaw. It’s a signal that your “traffic” is heavy, and it’s time to reduce it.
For a patient-friendly walk-through of why LDL-P can add clarity, see this explainer on why LDL-P matters. If your doctor also mentions non-HDL cholesterol, this internal overview of non-HDL cholesterol explained helps connect the dots.
What tends to raise LDL-P (and what improves it)
LDL-P often rises when the body produces more lipoproteins to move energy around, especially in insulin resistance. That’s why improving LDL-P is rarely about one magic ingredient. It’s usually about a pattern that lowers triglycerides, supports a healthy weight (if needed), and swaps the fat types that push particle production.
A few levers matter most:
A heart healthy diet pattern helps because it’s rich in fiber and unsaturated fats. On the other hand, frequent meals built around refined carbs, sugary drinks, and higher saturated fat can keep particles high. Alcohol can also raise triglycerides for some people, which can worsen particle patterns.
This is where “healthy food” stops being a slogan and becomes a routine: oats that show up five mornings a week, beans that find their way into lunch, olive oil replacing butter more often than not. Over time, that healthy nutrition rhythm supports better lipids and better energy.

Photo by Nataliya Vaitkevich
If you want a practical shopping approach that fits real life, this heart healthy foods guide is a solid companion to LDL-P goals.
A simple 3-week food focus to improve LDL particle number

Core foods that support better lipid patterns
A better LDL-P plan shouldn’t feel like punishment. Think of this as a 3-week “food focus” that makes the healthy choice the easy choice. It’s a healthy food diet built on repetition, not willpower.
Week 1: Build the fiber base (daily, not perfect)
Add one viscous fiber anchor each day: oats, barley, beans, lentils, chickpeas, chia, apples. Fiber helps reduce cholesterol absorption and often supports lower LDL-C and fewer atherogenic particles over time.
Keep it simple: oatmeal at breakfast, lentil soup at lunch, or chickpeas added to dinner.
Week 2: Swap the fats that drive particle production
Replace saturated fat sources with unsaturated fats most days. Use extra-virgin olive oil, nuts, seeds, and avocado more often. Choose fish or beans instead of processed meats when you can.
This is the “quiet” shift that many people underestimate.
Week 3: Tighten carb quality and protein choices
Aim for high-fiber carbs (whole grains, beans, potatoes with skin) and steady protein (fish, tofu, yogurt, poultry, legumes). Cut back on liquid sugar. If sweet drinks are daily, LDL-P progress often stalls.
A simple day that fits a heart healthy diet:
- Breakfast: oats with berries and chia
- Lunch: big salad with chickpeas, olive oil, lemon
- Dinner: salmon, roasted vegetables, quinoa
- Snack: plain yogurt with walnuts, or an apple

Meal prep that makes consistency easier
Food works better when movement supports it. A healthy living diet and exercise routine improves insulin sensitivity, often helping triglycerides and particle patterns. Keep it realistic: brisk walking most days plus strength training twice a week fits the idea of sports and exercise for long life.
Above all, treat this as nutrition to prevent illness, not a short-term fix. Retest when your clinician recommends it, often after several weeks of consistent changes.
Conclusion
LDL-C is the cholesterol “load,” but LDL particle number is the traffic count. When those disagree, LDL-P can explain why risk still matters. Ask about LDL-P when your family history, triglycerides, or metabolic health make the standard panel feel incomplete. Then commit to three weeks of fiber, better fats, and smarter carbs, a steady heart healthy diet that you can repeat. Your next lab draw should feel less like a verdict, and more like feedback you can use.


0 Comments