You can eat what looks like a clean healthy food plate, exercise a few days a week, and still get blood sugar levels that feel confusing. One number is “fine,” another is “borderline,” and suddenly you’re wondering what any of it means for your heart.
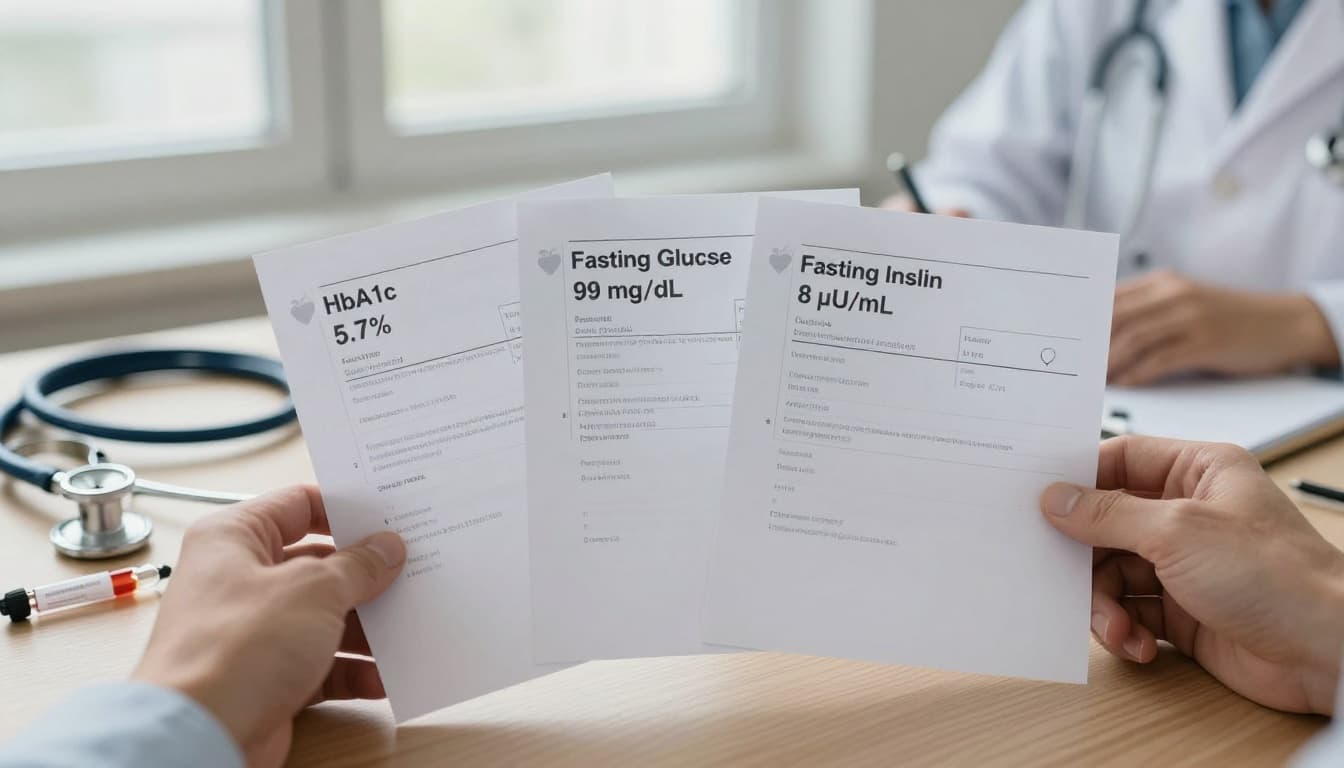
The comparison that trips people up most is A1c vs fasting glucose, key markers of metabolic health, because they can disagree even when you’re doing a lot right. These tests are essential for identifying prediabetes and Type 2 diabetes before they impact heart risk. Add fasting insulin to the mix, and it can feel like you’re reading three different weather reports for the same sky.
Here’s the plain-English meaning of each test, how each one relates to heart risk, and a realistic 2-week food focus you can repeat without turning life into a math problem.
A1c vs fasting glucose vs fasting insulin: what each test really measures
Think of your blood sugar like footprints in fresh snow. One test looks at today’s tracks, another looks at the whole week, and another looks at how hard your body worked to make those tracks.
| Test | What it measures | Time window | What it’s best at | What can blur the picture |
|---|---|---|---|---|
| A1c (HbA1c) | Sugar attached to red blood cells (glycated hemoglobin; Hemoglobin A1c) | ~2 to 3 months | Your longer-term average | Conditions affecting red blood cells (ask your clinician if you have anemia or recent blood loss) |
| Fasting glucose | Blood sugar levels after 8 to 12 hours with no calories | One moment | A quick snapshot | Stress, sleep, illness, late meals, and day-to-day swings |
| Fasting insulin | Insulin level after fasting | One moment | Clues about insulin resistance (helps calculate HOMA-IR score) | Lab ranges vary, and “normal” can still be high for you |
A1c tells you your average exposure. It’s like checking how much smoke has been in the room over months, not just whether you smell it right now.
Fasting glucose is your single morning number. It’s useful, but it’s also moody. A short night of sleep or a late, heavy dinner can push it up.
Fasting insulin doesn’t measure sugar; it reveals insulin sensitivity. If insulin is higher, it can mean your body needs to “shout” with more insulin to keep glucose steady. That often shows up before A1c climbs.
None of these tests is a personality test. They’re data points. The goal is to use them to shape a steadier routine, not to chase perfection. Clinicians look for optimal blood test ranges rather than just being in range.
What these tests can suggest about Cardiovascular disease (and why trends matter)

Your heart doesn’t care about one perfect morning. It reacts to repeated wear and tear, like a door hinge that squeaks after thousands of opens, not after one.
When glucose runs high too often, it can damage blood vessels over time and add to plaque buildup. That’s one reason A1c matters: it reflects the bigger pattern. Observational research has linked higher A1c to higher cardiovascular risk, even below diabetes levels in some groups (see this open-access review on A1c and incident heart disease risk).
Fasting glucose matters too. In a high cardiovascular-risk population without known diabetes, one study reported that HbA1c and fasting plasma glucose were similarly related to future cardiovascular risk (read the study summary on PubMed for HbA1c vs fasting glucose and CVD risk). That’s a useful reminder: if either marker is trending the wrong way, it’s worth attention.
Where does fasting insulin fit? It’s often treated as an early warning light for insulin resistance, a condition highlighted by indicators like the triglyceride-to-HDL ratio. Insulin resistance tends to travel with metabolic syndrome, including higher triglycerides, lower HDL cholesterol, higher LDL cholesterol, higher blood pressure, and extra visceral fat. These elements, plus poor glucose control reflected in elevated hsCRP as a marker of inflammation, all raise cardiovascular disease risk. As of early 2026, the strongest cardiovascular disease links in major guidelines still center on glucose measures (A1c and plasma glucose) plus the basics: blood pressure, lipids, smoking, sleep, and activity. Managing A1c and fasting glucose remains vital for those with Type 2 diabetes.
If you want a practical takeaway, use this rule: a single test is a photo, repeated tests are a movie. Bring your last few results to your clinician and look for direction, not drama.
For people who already have coronary artery disease, glucose markers can also help with prognosis. This paper in Diabetes Care discusses the prognostic value of fasting glucose and HbA1c in coronary artery disease.
A simple 2-week food focus for steadier numbers and a stronger heart
This isn’t a strict plan. It’s a 2-week reset that supports a heart healthy diet and steadier glucose without making you feel like you’re “on something.”
The core idea (keep it boring on purpose)
For 14 days, build most meals from three anchors: fiber + protein + unsaturated fat (while reducing saturated fat). That combo slows digestion, supports better satiety, and tends to reduce sharp spikes.
Use this as your simple “default plate”:
- A fiber base: beans, lentils, oats, barley, vegetables, berries, or whole grains
- A protein: fish, eggs, tofu, chicken, Greek yogurt, or legumes
- A fat: olive oil, nuts, seeds, avocado
It’s a healthy food diet pattern you can repeat on busy weeks because it’s flexible and aligns with a plant-based diet or a Mediterranean-style healthy eating approach. It also fits the bigger goal of healthy nutrition and “quiet consistency,” which is the kind that sticks.
Week 1: breakfast and snack cleanup (fast wins)
Pick one breakfast and repeat it most days. Repetition is a superpower.
Two easy templates:
- Oats with berries, nuts, and plain yogurt (or chia)
- Eggs (or tofu scramble) with greens and whole-grain toast, plus fruit
For snacks, keep it simple: fruit plus nuts, yogurt, or hummus with crunchy veg. This helps lower the “grab-anything” moments that usually mean ultra-processed carbs.
Week 2: lunch and dinner that don’t spike you
Choose two dinners and rotate them.
- Salmon (or sardines) with leafy greens, olive oil, and a bean side
- Lentil or bean bowl with chopped salad, avocado, and a whole grain
Need a guide for stocking your kitchen with repeatable staples? This heart-healthy foods guide lays out practical groceries and meal ideas that match this approach.
The small add-on that multiplies results
Pair your food changes with healthy living diet and physical activity habits: a 10 to 20-minute walk after one meal each day, and two short strength sessions per week (push, pull, squat, hinge, carry). This physical activity improves insulin sensitivity. It’s simple, it’s doable, and it fits the “sports and physical activity for long life” mindset.
Food is daily information for your body. Over two weeks, you’re not chasing a miracle, you’re practicing nutrition to prevent illness, supporting weight loss and stress management along with better A1c for long-term glucose control, the same way you brush your teeth: small steps, done often.
Conclusion
A1c, fasting glucose, and fasting insulin are three different lenses on the same system. A1c shows your longer pattern, fasting glucose shows today’s snapshot, and fasting insulin hints at how hard your body is working behind the scenes. Monitoring blood sugar levels through A1c, fasting glucose, and fasting insulin is a proactive way to avoid type 2 diabetes and cardiovascular disease. For heart risk, the most helpful move is to watch trends and build meals that keep your baseline calm. Try the 2-week focus, then re-check your routines and labs with your clinician and keep the parts that feel easy to live with. Healthy eating and consistent physical activity are the pillars of metabolic health, and consistency beats intensity when the goal is a longer, stronger life.

0 Comments